Endoscopic mucosal resection of large colorectal laterally spreading lesions
January 30, 2020
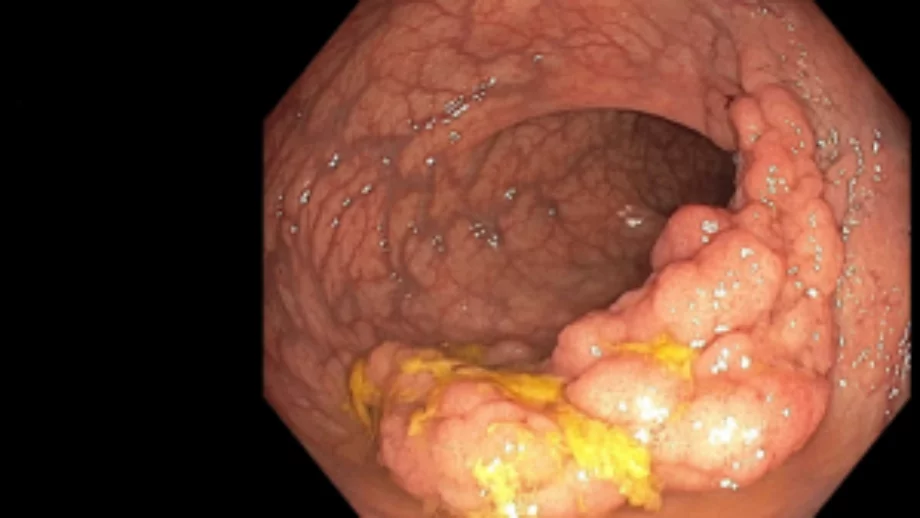
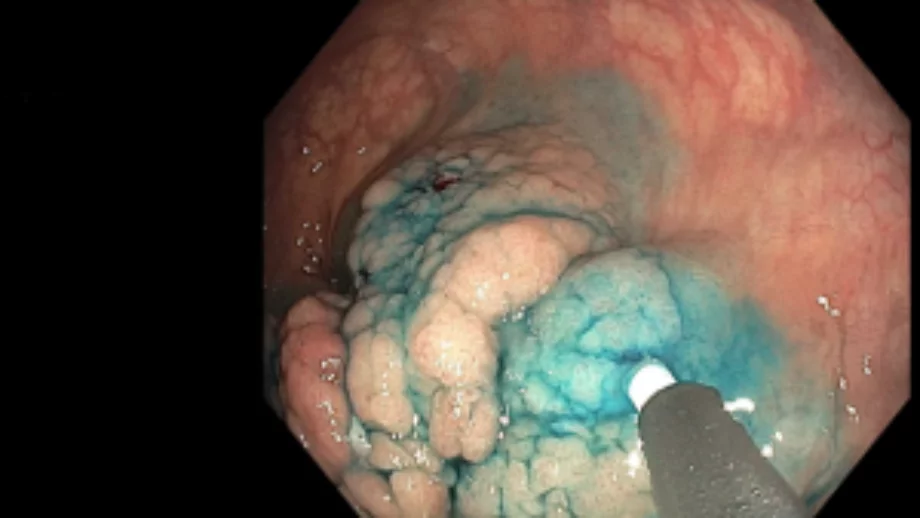
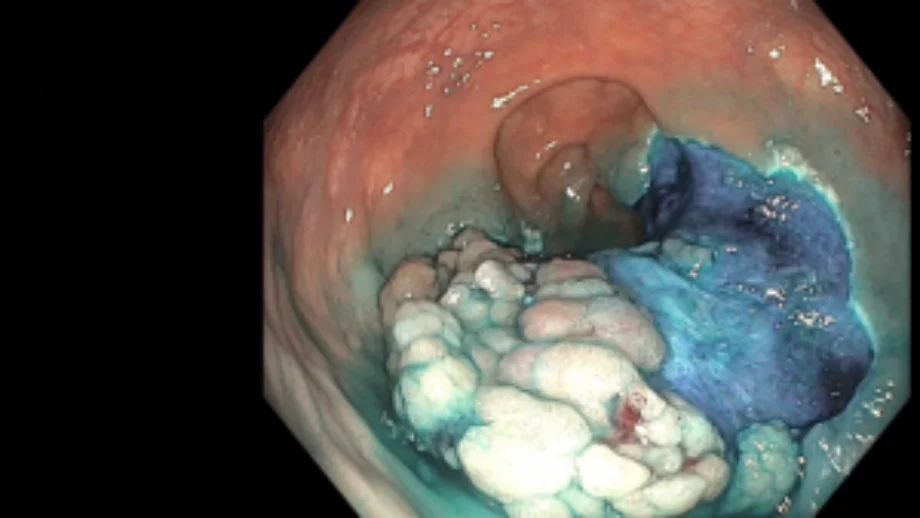
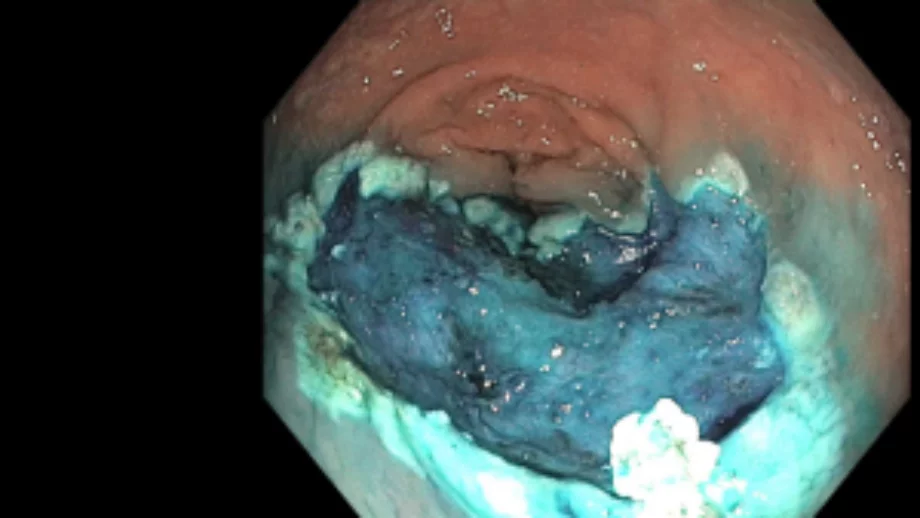
Most colorectal polyps are <10 mm in size, and easy to resect using standard polypectomy techniques. However, endoscopists may encounter large, flat, or sessile and ≥20 mm laterally spreading lesions (LSLs) which require special techniques and expertise for effective and safe resection. The technique of choice for most large LSLs is endoscopic mucosal resection (EMR), which has been shown to be more cost-effective and safer than surgical resection. These types of procedures take longer than routine ones and require additional training and experience to master. Below are principles, tips, and tricks that can help ensure successful resection and optimize outcomes.