Introduction
Acute pancreatitis is a common clinical problem globally. Pancreatitis can be interstitial or necrotic. Interstitial pancreatitis can result in acute pancreatic fluid collections (PFCs). These collections are generally homogeneous, do not extend into the pancreatic parenchyma, and tend to resolve spontaneously without intervention. Pseudocysts are generally seen a few weeks after pancreatitis (up to 4 weeks). These generally develop a wall, which matures in up to 4 weeks and has no or minimal necrosis. These tend to resolve spontaneously as well without intervention and would need intervention if they are symptomatic with a mature wall. When fluid collections are seen in a setting of acute necrotizing pancreatitis, they are called acute necrotic collections and can be intra- or extrapancreatic and do not have a defined wall. Walled-off necrosis (WON) is seen in a setting of pancreatic necrosis and is a heterogeneous collection of fluid and necrotic material, and typically develops a wall in about 4 weeks from the onset of acute pancreatitis.
Endoscopic ultrasound (EUS) and drainage of fluid collections has become a cornerstone for the management of symptomatic/infected WON or pseudocysts.
In this article, Dr. Sundeep Lakhtakia, Interventional Endoscopist at the Asian Institute of Gastroenterology, Hyderabad, India, shares his expert advice on endoscopic drainage of these fluid collections.
Dos
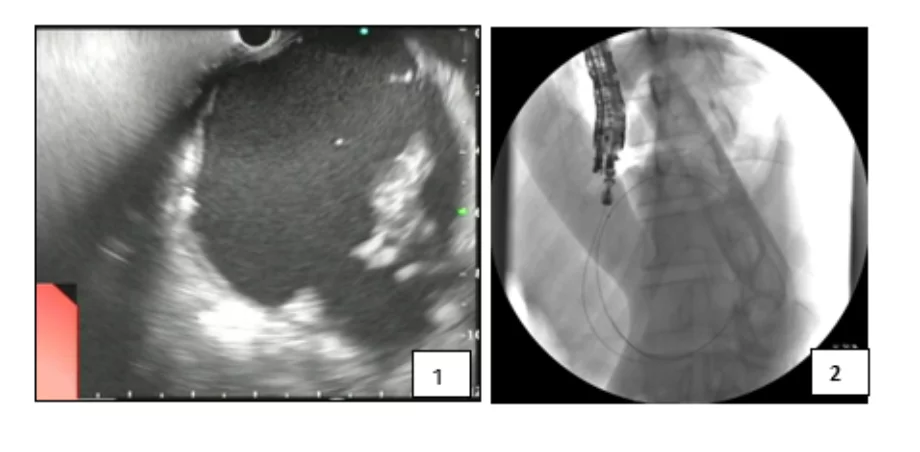
- Assess the PFC by EUS for: (Figure 1)
- maturity of wall
- content
- fluid alone (pseudocyst)
- fluid with solid debris (WON). Approximate percentage assessment of solid debris within WON
- interposing vessels, collaterals (avoid risk of bleeding from puncture site)
- size (largest in two dimension)
- wall thickness (<10 mm preferred)
- echotexture of remaining pancreas (normal in pancreatic cyst neoplasm)
- site of intended puncture
- stomach/duodenum/esophagus; if in doubt crosscheck with endoscopic view
- stomach – anterior wall (possible risk of free perforation) or posterior wall (minimal risk of perforation as lesser sac is a relatively closed space)
- position of echoendoscope – straight (easier passage of accessories) or curved.
- Puncture using 19-G EUS FNA needle at thinnest point without any interposing vessel.
- Aspirate about 10 mL of PFC fluid. Inspect it (clear or turbid fluid/pus). Send for analysis (amylase and microbiology culture).
- Guidewire – pass angle-tip 0.025” or 0.035” guidewire through the FNA needle and make 1–2 coils inside. Confirm position under fluoroscopy. (Figure 2)
- Fistula creation (between PFC and GI tract) by passing a co-axial over-the-guidewire 6-Fr cystotome.
- Dilate the fistula with balloon.
- Large-caliber balloon for plastic stents. 10–15 mm for stomach, 4–6 mm for esophagus, 6–8 mm for duodenum.
- Small-caliber balloon (4–6 mm) for passing assembly of non-LAMS.
- Plastic stents. Preferred for pseudocyst.
- Place two stents after placing two guidewires upfront. Use wide lumen or double catheter or second wire as loop-wire).
- Double-pigtail stent design preferred. Small caliber (7 Fr). Short stent (3–5 cm long). Mark the center of the stent with ink for accurate placement (prevent eccentric).
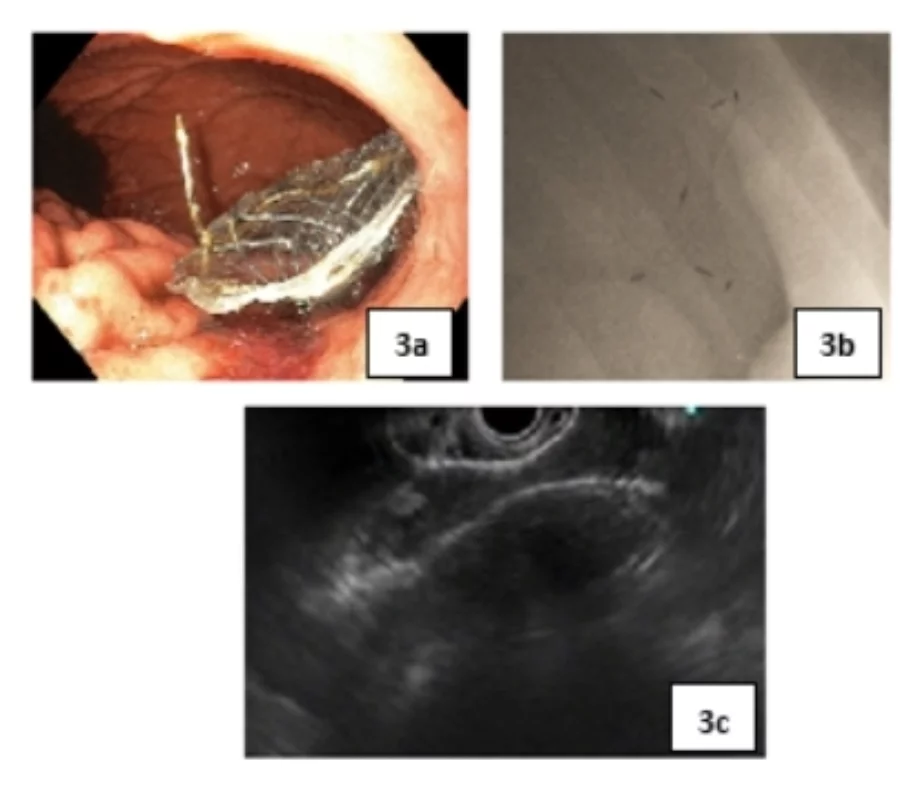
- Non-LAMS (lumen-apposing metal stent) deployment. Preferred for WON. (Figure 3)
- Internal half – use fluoroscopy and EUS view.
- External half – use fluoroscopy and endoscopy view.
- Ensure complete emptying of the stomach after drainage to prevent risk of aspiration.
- May place a double-pigtail plastic stent inside the non-LAMS to prevent migration, blockage of the lumen with loose debris in WON, and rubbing with resultant abrasion and bleeding from the collapsed back wall of the PFC against the LAMS edge.
- Nasocystic tube can be placed at index drainage or later for irrigating the PFC cavity to clean infected collections.
- Remove non-LAMS after 3–4 weeks of placement, after obtaining MRCP to exclude disconnected pancreatic duct (DPD) and resolution of PFC.
- In presence of DPD
- Non-LAMS – attempt exchange with plastic stent that are left indwelling permanently.
- Plastic stents – leave in situ indefinitely, to drain upstream pancreas.
1. EUS showing the PFC with mature wall and debris (WON)
2. Guidewire coiled one and a half times within the PFC
3. Final images after placement of Nagi stent: a) endoscopy; b) fluoroscopy; c) EUS